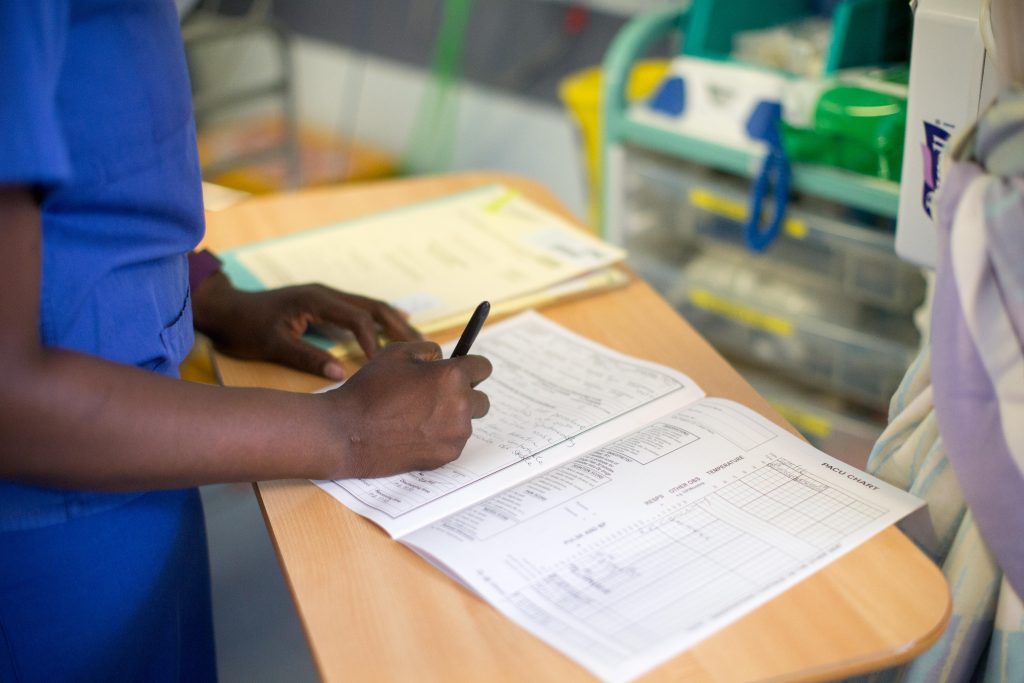
Nurses have a legal obligation to maintain accurate clinical records, and electronic documentation does not detract from the core principles involved.
The recent move towards electronic care documentation systems might create some logistical challenges for nurses, but it doesn't detract from the core principles of clinical record-keeping.
It is a legal obligation to ensure there are clear clinical records detailing patient care.
Nursing Times has just finished reviewing and updating its CPD learning unit on clinical record-keeping to help you keep up to date with a key element of the nursing role.
The Nursing and Midwifery Council's (NMC) Code is unequivocal in that nurses must keep clear and accurate records that are relevant to the professional's scope of practice which includes, but is not restricted to, patient records.
Nurses are no doubt aware of the role of clinical records in healthcare litigation and the need to maintain meticulous notes, but what might not be so obvious is the purpose given for documenting information. Literature suggests that over-focusing on clinical records in case of complaints or criminal or civil action can lead to the assumption that patient notes are maintained only to provide evidence of care carried out.
While it's correct that patient notes can be called upon as evidence, such a defensive view can skew approaches to record keeping by putting an emphasis on defending the care given rather than viewing records as a tool for providing appropriate care.
And though there may not be clear evidence that scrupulous clinical records improve patient care, indications from reviews by organisations such as the National Patient Safety Agency demonstrate poor clinical records do contribute to mistakes and substandard care.
To understand more about this area of professional responsibility and accountability, visit our clinical record-keeping learning unit.
After completing this unit you should be able to:
- Describe how to document clearly and safely
- Outline the role of record-keeping in ensuring clear measurable outcomes for patient care
- Illustrate the role of records in undertaking a root-cause analysis of an incident in healthcare and the importance of a clear “audit trail”
- Explain a nurse’s accountability and duty of care in relation to patient care and record-keeping
- Outline the role of records in complaints and civil court cases
- Describe how to use the SOAP (Subjective, Objective, Assessment, Plan) framework to record episodes of care
Visit this learning unit and the rest of our CPD zone here.
Don't miss more great clinical content from Nursing Times
NT Bitesize learning videos – helping you to organise learning to fit in with your schedule
Clinical zones – keep up to date with articles in your clinical subject or nursing role/setting
CPD zone – user-friendly online learning units on fundamental aspects of nursing
Journal Club – clinical articles with discussion handouts for participatory CPD
Practical Procedures – 'how to' guides and teaching materials for clinical procedures
Self-assessment – clinical articles with linked online assessments for bitesize CPD
Systems of Life – applied anatomy and physiology to support your practice
 Nursing Times Resources for the nursing profession
Nursing Times Resources for the nursing profession

Have your say
or a new account to join the discussion.